
How does diabetes affect how your insulin works?
Insulin is a hormone produced in the pancreas that regulates how much glucose is in your blood. It helps control blood glucose (sugar) levels by telling your liver, muscle, and fat cells to take in glucose from your blood, helping the glucose to be used in the body for energy. A lack of insulin or resistance to insulin can cause diabetes.
Insulin resistance is when cells in your muscles, fat, and liver don’t respond well to insulin and can’t easily take up glucose from your blood meaning your sugar levels rise. As a result of this, your pancreas produces more insulin. Overtime insulin-producing cells can become damaged or destroyed and stop producing insulin. This results in insulin deficiency whereby it leaves too much sugar in the blood and not enough in the cells for energy. When there is too much sugar in the blood, this can be known as hyperglycaemia.
Type 1 diabetes
Type 1 diabetes is a medical condition where your blood glucose level is too high because your pancreas cannot produce any insulin. Type 1 diabetes occurs when your immune system, the body’s system for fighting infection, attacks and destroys the insulin-producing cells of the pancreas.
People with Type 1 diabetes rely on insulin treatments to control their blood glucose levels, and they can take it through either a pump or an injection. People with Type 1 diabetes are usually diagnosed earlier in life and it is not known to be linked to age, weight or lifestyle factors.
Type 2 diabetes
Type 2 diabetes is a condition where the insulin your body makes does not work properly, or it cannot make enough. Many people with Type 2 diabetes are able to carry on without medications, but may need to make a few lifestyle changes such as:
- Increasing exercise
- Losing weight
- Changing their eating habits
However, if lifestyle changes do not have a great enough impact, then people with Type 2 diabetes may progress on to oral medications and/or injectables which can be taken through injections or pumps.
Types of insulin
There are 3 common types of insulin someone could be prescribed which are listed below:
- Rapid-acting/short-acting is usually taken before your regular meals to protect your glucose levels from rising while eating.
- Intermediate-acting is also known as background or basal insulin. This means it works throughout the day. It is often combined with rapid-acting or short-acting insulin.
- Long-acting is slower than intermediate insulin, but very similar in how your body processes it. It is often combined with rapid-acting or short-acting insulin.
The type you are prescribed will depend on your body’s needs.
Insulin administration and injection sites

You will be advised the best times to take your insulin by your healthcare professional. It’s important to adhere to these instructions to control your blood glucose levels.
Insulin doesn’t come in pill form because your digestive system would break it down before it had a chance to start working. Many people with diabetes will self-administer by injecting with a pre-filled pen. If you inject regularly you will need to vary the areas of your skin where you inject to ensure it is being absorbed consistently.
The ideal areas to inject are the parts of your body with a larger layer of fat, such as:
- Abdomen
- Thighs
- Buttocks
If you inject in the same place too often, your skin may start to become stiffer, this can often lead to it becoming lumpy. It can help to imagine a grid drawn onto your body so you can pick a different square to inject into each time. After some time, you’d need to start again at the first square you chose, but that should have fully healed by the time you’ve gone back to that area.
Some areas of your body will absorb insulin quicker than others so it’s important to keep track of this. Speak to your healthcare professional if you have any concerns about your injection sites and they will be able to advise you.
Storage advice
It’s important to store your insulin properly to make sure it is effective:
- Insulin should be stored in the fridge and away from heat. If you go out it will be useable at room temperature for short periods of time, but if you’re travelling it’s best to keep it in a cool bag.
- Keep it out of sunlight.
- Check the expiry date and don’t use it if it’s out of date.
How can Spirit Pharmacy help you?
Spirit Pharmacy specialises in helping people with diabetes. We can dispense your insulin prescriptions (along with your other medicines) and deliver it free of charge directly to your house in insulated environmentally friendly packaging to keep it cool. We also offer free diabetes education to all our customers and our pharmacists can help with any queries you may have.
Find out more about Spirit Pharmacy.

The weather is getting warmer and many of us are looking forward to enjoying life in the sun. However, it can be harder to control your diabetes in the summer.
Longer periods of inactivity in the sun can affect your diabetes control, making your blood sugar levels higher than normal. For those on insulin, it is important to know that it is absorbed faster from an injection in warmer weather which can put you at risk of hypoglycaemia (hypo). But as long as you are vigilant about your diabetes control, then there is no reason why you can’t enjoy yourself just like anyone else.
We have some top tips you can follow to ensure you can safely enjoy yourself and keep track of your diabetes in the summer!
Keep an eye on your levels
As with any change in your lifestyle, remember is to check your blood glucose levels and adjust your insulin dose accordingly. Make sure you’re regularly checking your levels and keep a sugary snack to hand, just in case.

Stay hydrated!
Everyone needs to stay hydrated in the warm weather, but especially if you have diabetes. People with diabetes get dehydrated more quickly in the heat. Not drinking enough liquids can raise your blood glucose levels which can lead to you urinating more, causing dehydration. Keep a bottle of water close by at all times, and drink regularly to help control your blood sugar levels.
Keep your meters and test strips out of the sun
The warmer weather can affect your meters and test strips just as much as it does you. Try to keep your meters and test strips as close to room temperature as possible and out of direct sunlight. (But don’t refrigerate them- the cold temperature has the same effect as warm temperatures against the meters and strips and can lead to misleading results.)

Keep your insulin cool
Insulin damaged by the heat will become cloudy. It can become grainy and sticky or maybe slightly brown (do not use insulin if it looks like this!)
Insulin is best kept in the fridge or a cool bag, just make sure it doesn’t freeze.
Always read the temperature guidance for your medication and test strips.
Take the usual good care of yourself!
Apart from having to check your blood glucose, you’re no different to anyone else enjoying themselves in the sun. Just keep hydrated, make sure you’re regularly applying sunscreen to exposed areas and take regular shade breaks to avoid dehydration, overheating or getting heat exhaustion.
How can we help?
Our pharmacists are trained to support you in managing your diabetes. Register with Spirit Pharmacy to receive your medication delivered direct to your door. You will have access to a team who can answer your queries and help you with any challenges you may be facing. You will also have access to online diabetes education if you would like it.
Register here
Walking is a great exercise for people with diabetes, who should pay particular attention to their foot health. It is light exercise, but also has excellent health benefits.
Walking can also help you take proper care of your feet and legs, which is vital if you have diabetes. It’s common knowledge that when you have diabetes, you’re at a much higher risk of developing problems with your feet. It can be a constant concern, worrying about losing a foot or a toe, but these aren’t inevitable side effects of diabetes. If you continue to maintain your blood glucose levels and have your feet checked regularly, you can avoid these problems and maintain good foot health.
How does diabetes affect your foot health?
Over time, poorly managed diabetes can cause nerve damage, otherwise known as diabetic neuropathy. This damage can cause tingling and pain in your feet and can lead to a loss of sensation, which is when other problems can arise. If you lose sensation in your feet, you won’t be able to feel things such as pebbles in your shoes or a blister on your foot, which can lead to cuts and sores which can become infected.
Diabetes can also affect your blood flow. If you have cuts or sores on your feet, your blood flow to these areas will be lowered, which means they’ll take longer to heal. If a cut or sore doesn’t heal, it can result in gangrene. In this case your doctor will refer you to hospital to have the infected tissue removed, but in extreme cases, gangrene can result in skin grafts and sometimes amputation.
What can I do to improve my foot health?
All of the cases listed are worst-case scenarios! If you manage your diabetes well, you are less likely to experience any extreme issues with your feet. It’s easy to manage your condition, especially by keeping on top of your medication, diet and regularly checking your feet.
How can I check my feet?

Spend a few minutes each day examining your feet. Look out for:
- Cuts and sores
- Fluid-filled blisters and swelling
- Ingrown toenails, where the edge of your nail is growing into the skin
- Athletes foot
- Warm spots
Take the time to treat these problems as they arise rather than leaving them. Most are easily resolved with a bandage or some over the counter treatment, but if the problem becomes consistent, then you can contact your GP or pharmacist for further support.
How can we help?
Our pharmacists are trained to support you in managing your diabetes. Register with Spirit Pharmacy to receive your medication. You will have access to a team who can answer your queries and help you with any challenges you may be facing. Confidential advice is available to all people registered with the pharmacy, as well as access to online diabetes education if you would like it.

While we know stress doesn’t cause diabetes, there is a link between stress and blood sugar levels, so it can affect your day to day handling of your condition.
Being diagnosed with diabetes or any chronic illness causes stress, that’s natural; it’s your body’s reaction to a new and challenging situation! You have to come to terms quickly with a diagnosis that changes your life, and this stress is only amplified when you feel like you or others don’t understand it.
Diabetes, stress and blood sugar
Stress isn’t healthy for anyone, diabetic or not. However, when you have diabetes, stress can have a specific impact on both your insulin and your blood sugar levels.
When the body becomes stressed, it releases stress hormones like cortisol and adrenaline into your system. In a person with diabetes, these hormones can make it harder for your insulin to work. When cortisol is released, it triggers your bodies natural ‘fight or flight’ reaction – this can cause your heartbeat and breathing to speed up. However, it also releases glucose stored in your liver into your blood so the energy can get throughout your system. In a person with diabetes, the pancreas struggles to keep up with the high demand for insulin, causing insulin resistance. As the energy can’t get into the cells, this causes your blood sugar levels to rise.
If your blood sugar levels rise too much, this can cause a ‘hyper’ (hyperglycaemia) which can lead to you feeling thirsty, lethargic and give you a headache. If the stress doesn’t go away, it can keep your blood sugar levels high and put you at a higher risk of other diabetes complications, as well as affecting your day to day mood and how you look after yourself and your condition.
But don’t worry! There are plenty of things you can do to take the pressure off.
Stress busters

Putting yourself first should always be top of your priority list, but it’s easy for that to take a backseat when you’re feeling stressed. When you’re stressed, take control of the aspects you can change about your life and learn to say no to things that will unnecessarily add to your load. Jot in a bit of time in your diary for some well needed you time. Spend time with your friends and family, go on a nice walk, light a candle, listen to soothing music. Whatever it may be, just take some time to step back and relax. Look at this page to get some tips on how you can relive stress.
The bottom line is stress will always find a way to wiggle itself into your life, but by making time for things that can relieve it, it can become much more bearable for you in your day to day life.
We can help
It doesn’t matter whether the stress you’re feeling is related to diabetes or not; it’s getting the support you need to manage it that is important. Our pharmacists are trained to support you in managing your diabetes. Register with Spirit Pharmacy to receive your medication. You will have access to a team who can answer your queries and help you with any challenges you may be facing because of stress. Confidential advice is available to all people registered with the pharmacy, as well as access to online diabetes education if you would like it.

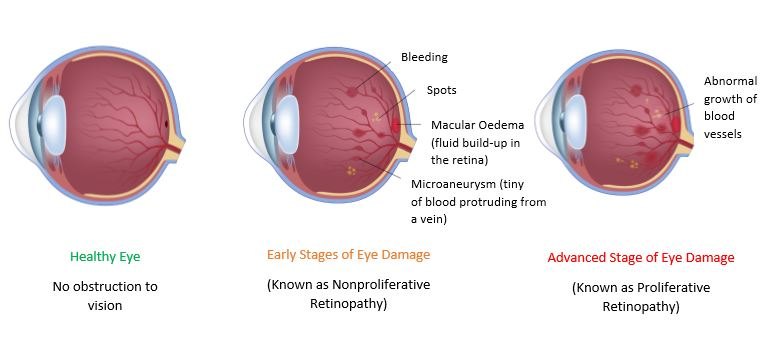
People who have diabetes are at a higher risk of developing eye complications, specifically known as diabetic retinopathy. The images above show how diabetes-related eye problems can affect your vision. However, by taking an active role in managing your blood glucose you can reduce your risk of this happening.
What is diabetic retinopathy?
Retinopathy is damage to the retina, the innermost layer in the eyes. This can lead to loss of vision. Over time, high levels of glucose in the blood can damage the retina. The retina is a sensitive layer at the back of the eye that has many tiny blood vessels. These blood vessels can become damaged and leak. New blood vessels form in the retina to compensate. These blood vessels can easily leak too.
Imagine how easy it is to drink water through a thin straw. Now imagine how much harder it is to drink a thick milkshake through the same straw. Not easy at all! In the long term, these damaged blood vessels cause problems with vision and if left untreated can stop you seeing.
The longer you have unmanaged diabetes, the more likely you are to experience eye problems.
Eye health
Regular checks and general awareness
If you have diabetes, once a year, you will be invited to a free NHS retinopathy screening. It is essential that you attend these appointments. When you attend someone will put a special eye drop into your eyes. These eye drops dilate your pupil. For that reason take someone with you. Do not drive to your appointment as you will not be able to drive for a short while after. And don’t forget your sunglasses as your eyes will be a little sensitive to light after the test.
A picture of the back of your eye will be taken to detect any early signs of diabetic retinopathy. If required, you may need to see an eye specialist. Some people need eye treatment to preserve their vision. One treatment is known as laser therapy. This is where a beam of light makes tiny burns on the retina to stop blood vessels leaking and reduces the growth of new vessels.
But don’t wait for an appointment if you think you have a problem. Make an appointment with your healthcare professional if you experience:
- Sudden blurred vision
- Changes in normal vision
- Dark areas in normal vision
- Spots or blobs floating inside your eye
What can I do to prevent diabetic retinopathy?

There are many things you can do to help keep your eyes healthy and help prevent diabetic eye complications.
- Manage your blood glucose — Taking control of blood sugar can slow down or stop the progress of eye disease. If you haven’t noticed any problems yet, there is no reason why your eyes should be any worse than people who do not have diabetes. Check your blood sugar levels as advised by your healthcare professional.
- Take your meds — Remember to take any medication you have been prescribed to help manage your diabetes. Blood pressure and cholesterol levels should also be kept under control.
- Stop smoking — We all know that smoking is bad for our health, but in people with diabetes, it increases the risk of developing eye complications. Speak to your healthcare professional or visit NHS support.
- Stay healthy — Healthy eating and regular exercise will help keep your blood sugar levels stable and help with weight control. Find what works for you!
- Attend your regular check-ups, including any eye screening appointments.
Spirit Pharmacy is here to help
Our pharmacists are trained to support you in managing your diabetes. Register with Spirit Pharmacy to receive your medication. You will have access to a team who can answer your queries and help you with any challenges you may be facing because of poor eyesight. Confidential advice is available to all people registered with the pharmacy, as well as access to online diabetes education if you would like it.
Sign up to Spirit Pharmacy by clicking the Register button at the top of the screen.