Whether you have Type 2 diabetes, or know someone who does, being aware of what your levels of blood sugar should be and how this can affect your body, is very important. This blog is here to help you understand everything you need to know about blood sugar levels, written by our Medical Director.

What level of blood sugar is normal range?
If you have Type 2 diabetes, a normal range for your blood glucose levels is:
- before meals: 4 to 7mmol/l
- two hours after meals: less than 8.5mmol/l
If the term mmol looks a bit strange to you, don’t worry! mmol/l stands for millimoles per litre and a mole is a scientific unit often used to measure chemicals.
What are common causes of low blood sugar levels?
Low blood sugar levels, also known as hypoglycaemia or a ‘hypo’ is when your blood sugars are below 4mmol/l. It is not always known why hypos may happen, but there are some common causes that make them more likely. These include:
- Missing or delaying a meal or snack.
- Not having enough carbohydrates at your last meal.
- Doing a lot of exercise without having extra carbohydrates or without reducing your insulin dose (if you take insulin).
- Taking more insulin (or certain diabetes medication) than you need.
- Drinking alcohol on an empty stomach.
It is important that you know how to recognise a ‘hypo’ and how to treat it swiftly, as well as knowing how to prevent them in the future. For more information, read our alternative blog post.
What are common causes of high blood sugar levels?
High blood sugar levels, also known as hyperglycaemia or a ‘hyper’ is when you have a higher-than-normal amount of glucose in your blood. This is usually above 7 mmol/L before a meal and above 8.5 mmol/L two hours after a meal. Hyperglycaemia can happen because the body either cannot produce enough insulin to process the sugar in the blood or it cannot use the insulin effectively enough. Some of the common causes for hyperglycaemia are:
- You may have missed a dose of your medication.
- Have eaten more carbohydrates than either your body or medication, or both, can cope with.
- You are stressed.
- You are unwell from an infection.
- You have over-treated a hypo.
For more information on hypoglycaemia and hyperglycaemia, read our blog post; Blood Glucose Levels: Hypoglycaemia vs. Hyperglycaemia.
Do I need to monitor my blood sugar if I have Type 2 diabetes?

Not necessarily – not everyone with Type 2 diabetes needs to check their sugar levels. However, if you take certain medications, such as insulin or sulphonylureas, checking your blood sugars is a vital part of living with diabetes. By doing this, it can help you work out if you need to take more medication or when you need to eat something.
If you’re unsure about any of this, please speak with your healthcare professional and they will be able to help you with any questions you may have.
Are blood sugar levels affected by stress?
When we become stressed, our body releases two stress hormones known as cortisol and adrenaline. These hormones are what give you an energy boost for a ‘fight or flight’ response. However, these hormones can make it harder for insulin to work properly and when insulin resistance occurs, energy can’t get into your cells and therefore, your blood sugar levels rise.
Stress can also lead to overeating, which could also be a factor as to why your sugar levels rise – this in the long term can also lead to weight gain which is a known risk factor for developing Type 2 diabetes. For 9 ways to manage stress for better blood glucose control, read our blog.
If you have any further questions about any of the topics discussed above, please contact your diabetes registered healthcare professional.
—-
At Spirit Pharmacy, we’re here to help people who live with diabetes get access to their medicines, helpful items, and expert advice. We offer a friendly NHS prescription free home delivery service, alongside lots of additional services and support, especially tailored for people living with diabetes.
Please note, this article is not intended to be individual healthcare advice. Always follow specific advice relating to your condition given to you by your doctor, pharmacist, diabetic nurse, or dietician.
*Information correct at time of issue – March 2022
If you’re diagnosed with diabetes (whatever type), it’s important to be aware of how this can affect your body. However, the amount of information to take in when you have diabetes can sometimes be overwhelming, which is why we’ve started a Doctor Q&A series which answers some popular questions about diabetes.
Our Medical Director, Richard, has taken some time to outline the key points of how diabetes can affect your feet. Read more below.

Does diabetes affect your feet?
Having diabetes means you’re at much greater risk of developing foot problems. This is because, when your sugar levels are too high, this can damage the feeling in your feet. High sugar levels can also affect your circulation meaning you are getting less blood supply to your feet. Without a good blood supply, you may have problems with cuts and sores healing, and you may also get cramps and pain in your legs or feet.
It’s really important to check your feet regularly and attend your annual foot check with your healthcare professional, as most foot problems can be prevented with good foot care and regular checks. However, if you don’t get these foot problems treated, they could lead to foot ulcers, infections and, at worst, amputations.
Will diabetes cause your feet to swell and why?
Persistent high blood glucose levels (hyperglycaemia) can damage the lining of smaller blood vessels. This damage can result in poor blood circulation and in turn, this can result in swollen feet and ankles. This happens when your blood doesn’t circulate properly and fluid gets trapped in certain parts of your body, such as the legs, ankles, and feet. This excess fluid that builds up in the body tissue which is known as oedema.
What can you do to prevent diabetic foot problems?
Preventing foot problems is essential if you have diabetes. Undertaking regular self-checks and attending your annual foot check are the best way to prevent common foot problems from occurring.

Here are some ways that you can protect your feet in further detail:
- Check your feet daily by doing it yourself or asking someone to help you. You/they should be looking for any changes or injuries. If you’re checking on yourself and cannot lift your legs, use a mirror to look at the soles of your feet.
- Clean your feet daily: Keep your feet clean and dry thoroughly (including between your toes).
- Wear supportive shoes and socks: Do not apply socks so snugly that they restrict blood flow and make sure your shoes are the correct size and are wide enough.
- Trim nails carefully: Trim toenails straight across, keeping them short and using a nail file for the edges.
- Protect feet from extreme temperatures: Exposure to extreme hot and cold can damage your feet. It’s also a good idea to avoid walking around bare foot.
- Attend your annual foot check: Regular examinations by a healthcare professional are key to preventing infections, amputations, and severe deformities.
- Control blood sugar: Uncontrolled blood sugars increase the risk of neuropathy and foot problems, so keeping your blood sugar levels in check is going to help.
- Avoid smoking: Smoking can affect the blood supply to the tissues, which can make foot problems worse in people with diabetes.
If you have any further questions about any of the topics discussed above, please contact your diabetes registered healthcare professional.
—-
At Spirit Pharmacy, we’re here to help people who live with diabetes get access to their medicines, helpful items, and expert advice. We offer a friendly NHS prescription free home delivery service, alongside lots of additional services and support, especially tailored for people living with diabetes.
Please note, this article is not intended to be individual healthcare advice. Always follow specific advice relating to your condition given to you by your doctor, pharmacist, diabetic nurse, or dietician.
*Information correct at time of issue – March 2022
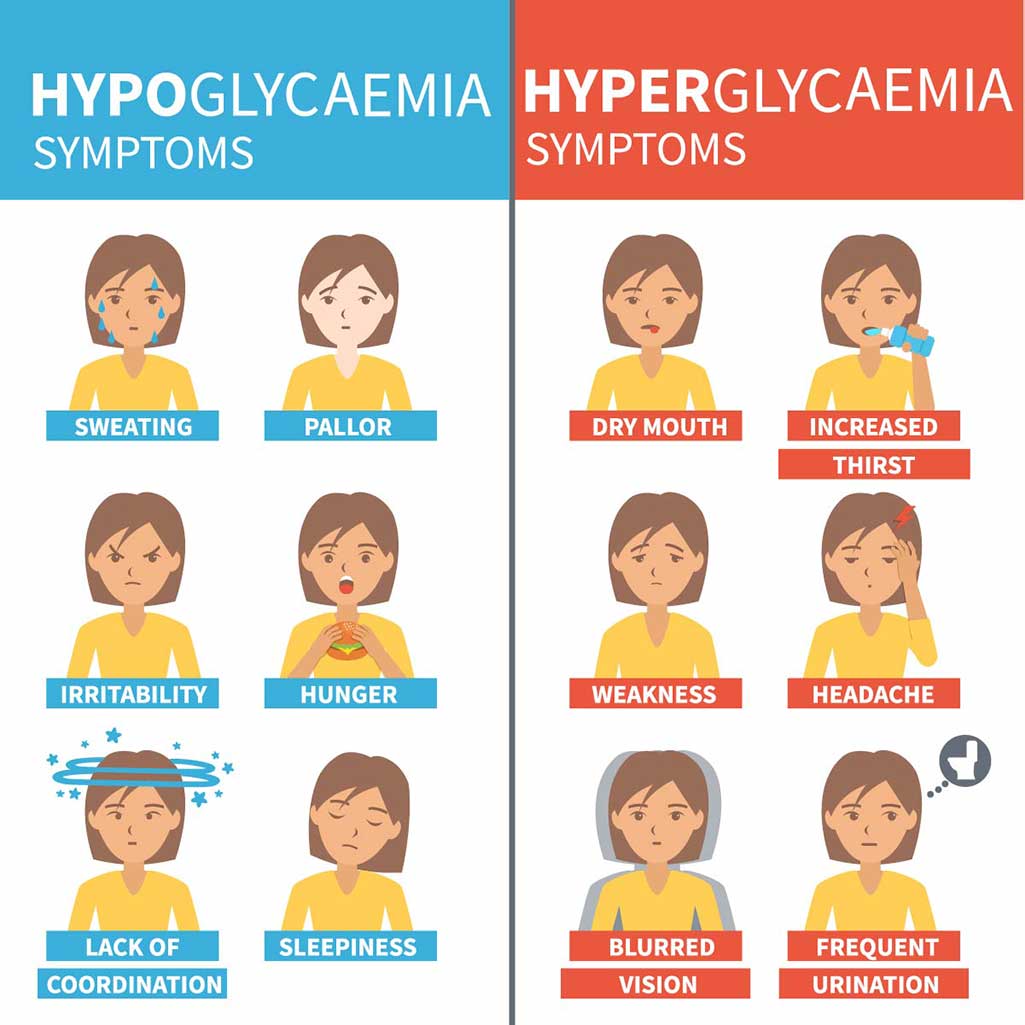
If you don’t have diabetes, you might have heard the terms ‘hyperglycaemia’ and ‘hypoglycaemia’ around (sometimes abbreviated to a ‘hyper’ or a ‘hypo’) and if you do live with diabetes, you might have even experienced them.
When you have diabetes, it’s important to know about these as they’re linked to your blood glucose levels. It’s vital to know the differences and what symptoms you might experience, so that you know how to treat them and understand why it might happen to you so you can prevent them in the future – and this blog is here to help you do just that.
What is hypoglycaemia?
Hypoglycaemia (sometimes called a ‘hypo’) is when your body has a low level of blood glucose, usually below 4 mmol/L. When your blood sugar is too low, your body does not have enough energy to work as well as it should.

What are the causes of hypoglycaemia?
- You may have missed or delayed a meal or snack.
- You might not have had enough carbohydrates at your last meal.
- Doing a lot of exercise without having extra carbohydrates or without reducing your insulin dose (if you take insulin).
- Taking more insulin (or certain diabetes medication) than you need.
- Drinking alcohol on an empty stomach.
Insulin and some other diabetes medications can make you more likely to have a hypo. If you’re unsure whether the treatment you’re on is likely to cause hypos, please check with your diabetes healthcare professional.
What are the symptoms of hypoglycaemia?
If you’re having a hypo, you may have warning signs that your blood glucose levels are too low, such as:
- Feeling shaky and disorientated.
- Feeling anxious.
- Suffering from headaches.
- Feeling hungry.
- Having a lack of concentration.
- Your vision may be blurred.
- Losing consciousness.
- Feeling higher levels of aggression.
- Falling into a coma.
- Sweating more than usual.
What is the treatment for hypoglycaemia?
First of all, it’s important to not panic. However, you will need to treat a hypo straight away. Don’t worry though, you can do this by eating food or having a drink that contains sugar.
This could be:
- Four or five glucose or dextrose tablets.
- Five jelly babies.
- A small glass of a sugary (non-diet) drink.
It’s important to know why the hypo has happened so you can try to stop it happening again. Learning why they happen is the best way to stay healthy, so if you’re unsure about why it may have happened, please speak to you doctor or nurse.
What is hyperglycaemia?
Hyperglycaemia is when you have a higher-than-normal amount of glucose in your blood. This is usually above 7 mmol/L before a meal and above 8.5 mmol/L two hours after a meal.

What are the causes of hyperglycaemia?
- You may have missed a dose of your medication.
- You might have eaten more carbohydrates than either your body or medication (or both), can cope with.
- You may be feeling stressed.
- You are suffering from an infection so may be unwell.
- You have over-treated a hypo.
What are the symptoms of hyperglycaemia?
You may have warning signs that your blood glucose levels are too high and experience symptoms such as:
- You may feel thirstier than usual.
- You might pass urine more often – particularly at night.
- You may feel tired or lethargic.
- Your vision may become blurry.
- You might suffer from headaches.
- You may have thrush or other recurring bladder and skin infections.
- You might lose weight.
What is the treatment for hyperglycaemia?
To treat hyperglycaemia, your blood glucose will need to be lowered to a normal amount. If you are feeling unwell, it’s important to not ignore it, make an appointment to see a doctor or nurse and ask to be seen within 24 hours.
If you’re unsure of any of the content we’ve covered above, please speak with your diabetes healthcare professional. If you have Type 2 diabetes and feel like you could benefit from being in a Facebook support group, we run a Daily Type 2 Diabetes chat club where people with similar experiences can share advice, tips and support one another. If you’d like to, please join here.
When you register as a patient with us, you’ll receive our free Live Well With Diabetes welcome pack, printed monthly trackers for you to stay on top of your progress, foot care guides, and so on. You can easily register with us on our website.
At Spirit Pharmacy, we’re here to help people who live with diabetes get access to their medicines, helpful items, and expert advice. We offer a friendly NHS prescription free home delivery service, alongside lots of additional services and support, especially tailored for people living with diabetes.
Please note, this article is not intended to be individual healthcare advice. Always follow specific advice relating to your condition given to you by your doctor, pharmacist, diabetic nurse, or dietician.
*Information correct at time of issue – March 2022
Living with diabetes can be a stressful experience and sometimes it can feel overwhelming. Whether you’re on several medications, or you’ve been told by your diabetes nurse that you need to change several aspects of your lifestyle, it can all feel a bit much to handle.
So, why not start with an extra 1%? We’ve outlined some tips below which you can use to start taking small steps to improve the management of your diabetes.
Exercise

If you’re trying to incorporate more movement into your life, but you’re not ready to go to an exercise class or take up running, there are much smaller changes you can make which will still have a benefit! Here are some ideas:
- Park slightly further away from the shop in the car park so you walk that little bit further
- Download an app or use a watch to monitor steps – if you don’t want to go out, you could walk on the spot whilst watching TV to get a few more steps in
- Set an alarm on your phone once every hour to get up and walk around the house for a few minutes, or go and get yourself a drink
- Walk around the house, or go for a walk outside whilst you’re on the phone
- Add steps into your chores e.g., if you’re taking clean clothes upstairs, do it in two trips to get more steps in
- If you can and it’s safe to do so, take the stairs instead of the escalator or lift
Food

Eating habits are often something that needs to be altered when trying to improve management of diabetes. However, there are many small food swaps that you can make that still keep your meals delicious whilst being slightly leaner or lower in carbs or sugar.
From Smokey Chipotle Chilli Nachos to Southern Fried Chicken and Sticky Cauliflower Wings, we have a whole host of delicious recipes available in another blog. Read our ‘fake-away’ recipes here.
Diabetes UK also have useful resources and ideas for healthy snack swaps and DIY takeaways. Read more about their recipes here.
Sleep

A good night’s sleep supports your body and mind to tackle day-to-day life and stress more easily. If you are tired, this can impact your patience and you might get agitated more easily, which can then increase your stress.
If your sleep (or lack of) is impacting your stress levels, this can affect your blood sugar levels as cortisol (the stress hormone) and adrenaline are released into the bloodstream. making it harder for insulin to work properly, this is known as insulin resistance. If you’re dealing with a lot of stress in your life, read nine ways to reduce stress for better blood glucose control.
Lack of sleep can also impact things such as your ability to remember to take your medications or have the energy to eat a balanced diet. Most adults need 7 to 9 hours of sleep each night and through practicing certain tactics, this can help to improve your quality of sleep. Some suggested ideas include:
- Ensure your bed is comfortable for you. Whether that’s making sure you’re warm with blankets, or making sure your pillows are at the correct and comfortable height
- Practice a consistent night-time routine. Whether that’s reading before you go to sleep, avoiding screens for the last half an hour of your evening or enjoying a relaxing hot drink
- Stick to a consistent time to go to bed so your body learns the routine
- Try and incorporate exercise into your daily routine as this may make you feel more tired and find it easier to sleep
Feet

You have a higher risk of developing foot problems when you have diabetes which can increase the risk of nerve and circulation problems, potentially leading to more serious problems such as ulcers, infections and amputations.
Don’t worry though, most foot problems are preventable and with good, regular foot care, these problems can be avoided.
To make sure you’re keeping on top of your foot health, a small step you can take is five minutes every few days to look for a change of feeling in your feet. This could include:
- Tingling or pins and needles
- Burning or hot feet
- Changes in the shape of your feet
- Build-up of hard skin or loss of feeling in your toes or feet
For extra steps that you can take in your daily routine, here are a few ideas:
- Do not walk around barefoot
- Avoid extreme temperatures of hot and cold – you might not know if you have hurt your feet if you have no feeling
- Do not use corn plasters or blades to remove hard skin – speak to your doctor or nurse if you have a problem. They may suggest you see a podiatrist
- Make sure when you buy new shoes that they are broad and supportive enough
- Check inside your shoes before you put them on. Look for sharp objects that may be inside. These could rub your feet and cause a blister
- Try to keep good diabetes control as this can help prevent foot problems
- If you smoke, the best thing you can do is stop. Smoking affects your circulation. This can increase your risk of developing serious foot problems.
For more information about foot care for those with diabetes, check out our overview of foot health for people with diabetes.
At Spirit Pharmacy we’re here to help people who live with diabetes get access to their medicines, helpful items, and expert advice. We offer a friendly free NHS home prescription delivery, alongside lots of additional services and support, plus a free Live Well With Diabetes welcome pack with your first delivery.
Please note, this article is not intended to be individual healthcare advice. Always follow specific advice relating to your condition given to you by your doctor, pharmacist, diabetic nurse, or dietician.
*Information correct at time of issue – February 2022
It can be difficult to know whether you’re entitled to free prescriptions, especially if you could potentially be exempt for a few reasons. However, did you know that if you are prescribed insulin or other medicines to manage your diabetes, you are entitled to free NHS prescriptions?
We’re here to give you a little more information about how you can claim your free prescriptions in England and, if you don’t use medication to manage your diabetes, how you might still be able to make use of prescription charge exemptions.
How do I claim my NHS medical exemption certificate?
If you take medications for your diabetes, you could get a medical exemption certificate provided by NHS England, also known as an NHS exemption card.
What do I need to know about a medical exemption certificate?
- It entitles you to free NHS prescriptions only
- It doesn’t cover dental treatment or help with other health costs
- It should be shown when you collect a prescription
- It is valid for five years (or until your 60th birthday, whichever is sooner)
- It will fall under the option of ‘has a valid medical exemption certificate’ on your prescription
If you’re entitled to a medical exemption certificate, your doctor will give you an application form. However, if this is not the case and you think you might be entitled to one, please contact your GP.
Find out more from the NHS.

Can I get free prescriptions if I don’t use medicines to manage my diabetes?
If you’re not prescribed insulin or other medicines to manage your diabetes, you will not be able to apply for a medicine exemption certificate (unless you have another medical condition which means you’re exempt). However, there are other exemptions which mean your NHS prescriptions could still be free. Some examples for NHS in England include:
- Age – If you are over 60
- Are pregnant or have had a baby in the previous 12 months and have a valid maternity exemption certificate
- Hold a valid war pension exemption certificate and the prescription is for your accepted disability
- If you receive Income Support or income-based Jobseeker’s Allowance
Read the full NHS prescription exemption list on the NHS website.
Please note that the age bracket of over 60 years of age may change to over 66 in the near future. So, if you’re between the age of 60 and 66 and not exempt for any other reason than your age, you may start having to pay for your prescriptions if this change is made. However, if you’re on medication for diabetes, or have any other exemptions, this age change will not affect you as you’re exempt for other reasons.
Please note that the Government consultation to increase the age bracket from 60 to 66 is still in process and for now, the age bracket remains at over 60 to be able to get a free prescription. Find out more and find updates on Gov.uk.
How can I check if I’m entitled to free NHS prescriptions?
If you would like to check whether you’re entitled to an NHS prescription exemption, you can check using NHS’ easy prescription exemption checker. However, if you’re ever in doubt, please get in touch with your GP for further questions and any advice on applying for a medical exemption certificate.
At Spirit Pharmacy we’re here to help people who live with diabetes get access to their medicines, helpful items, and expert advice. We offer a friendly free NHS home prescription delivery, alongside lots of additional services and support, plus a free Live Well With Diabetes welcome pack with your first delivery.
Please note, this article is not intended to be individual healthcare advice. Always follow specific advice relating to your condition given to you by your doctor, pharmacist, diabetic nurse, or dietician.
*Information correct at time of issue – January 2022

In our second edition of our Diabetes Treatment “Need To Know” series, Roma, our expert pharmacist talks us through a very common diabetes medication – metformin.
Why may a person with diabetes be prescribed metformin?
If you are diagnosed with Type 2 diabetes, your doctor will initially advise you to make diet and lifestyle changes. This is to help lower your blood sugar levels; in other words, eating a healthy, balanced diet and increasing the amount of exercise you do.
Your blood sugar levels will then be monitored again after a few months and if they are still higher than the recommended levels, then you may need medication to help decrease your blood sugar levels. So, metformin is usually the first choice of medication that is prescribed for Type 2 diabetes if diet and lifestyle changes have been insufficient.
What should people expect to happen when they first start taking metformin?
To understand this, it would be helpful to look at how metformin actually works. Metformin helps to reduce the amount of sugar that your liver releases into the body and it also helps the body’s insulin work better. Both mechanisms result in a drop in blood sugar levels to a healthy level.
This means that if you have been experiencing any symptoms of diabetes, such as increased thirst and urination, feeling tired, or blurred vision, then these symptoms will resolve as you take metformin and your blood sugar levels are controlled. You may possibly experience some side effects – indigestion being the most common.
Is metformin known by any other name, and are there different types?
There are two types of metformin: standard-release and slow-release. Standard-release tablets will release metformin into your body straight away and it will work quickly. However, this means it will get used up quickly too, so you may have to take it several times a day. Slow-release tablets release metformin gradually into your body throughout the day so taking it once a day is usually sufficient.
A liquid form of metformin is also available for those who may not be able to swallow tablets.
Metformin can come as a standard generic medication, or it can be known by the following brands: Bolamyn, Diagment, Glucient, Glucophage, Metabet and Sukkarto.
What are your 3 top tips for people to ensure they take their metformin effectively?
Firstly, take your metformin with or after a meal. While this will help reduce any side effects, it is also a good way to remember to take medication. If you take it everyday with breakfast, then you will automatically reach out for your metformin every morning with your food.
Secondly, speak to your doctor if you experience any side effects, especially indigestion. They will be able to provide you with options to overcome this.
And thirdly, metformin can very rarely cause more serious side effects. Watch out for shortness of breath, muscle cramps or feeling extremely cold.
I’ve heard metformin can give you a bad stomach. Should I be worried?
Taking metformin with or after a meal greatly reduces the chances of a bad stomach, so try this first. Your doctor will also recommend slowly increasing your dose of metformin within the first few weeks depending on your blood sugar levels.
If you still get indigestion, speak to your doctor and they can consider switching you to a slow-release metformin. This formulation is known to have a significantly lower occurrence of indigestion.
If that doesn’t help, then your doctor may consider prescribing you an alternative diabetic medication to suit your needs. There are several solutions available, so don’t worry.
Thanks for lending us your expertise, Roma. Look out for our next edition, our “need to know” series covers diabetes treatments and medications.
At Spirit Pharmacy we’re here to help people live well with diabetes. We offer free NHS prescription delivery, expert support, plus a free Live Well With Diabetes welcome pack with your first delivery.
Please note, this article is not intended to be individual healthcare advice. Always follow specific advice relating to your condition given to you by your doctor, pharmacist, diabetic nurse, or dietician.

We know that cooking can be time consuming and the temptation to treat yourself to a takeaway on the weekend is strong. Try our amazing ‘fake-away’ recipes instead of a takeaway, from a warming curry to a spicy chilli or finger licking chicken to fragrant Chinese. Our recipes will ensure that you will be able to enjoy amazing food, whilst choosing a healthier option.
Ultimate Curry Night
This ultimate curry night recipe uses high-protein chicken dhansak curry with lentils, cauliflower rice, and a mushroom bhaji accompaniment which makes this the perfect weekend alternative to an Indian takeaway and guaranteed to warm you up.
This meal is high-protein, low GI and provides 426 kcal per portion.
Ingredients (serves 4):
For the Cauliflower Rice – 1 large head cauliflower
For the Mushroom Bhaji – 400g white mushrooms, 1 medium onion, 1 tsp tomato paste, 2 cloves garlic, 1 tsp turmeric, 1 tsp cumin, handful of coriander
For the Chicken & Lentil Curry – 4 chicken breasts cut into chunks, 1 medium onion, 100g red lentils, 2 cloves of garlic, 1 thumb sized piece of ginger, chilli to taste, 1 tsp turmeric, 1 tsp garam masala, handful of coriander, 400g tin of tomatoes, 500ml chicken or vegetable stock
Nutritional Information (per serving)
Calories 426, Fat 6.1g, Carbs 38.4g (9g of which sugars), Fibre 14.6g, Protein 59.3g
For the Cauliflower Rice
- Wash and thoroughly dry cauliflower, then remove all greens.
- Cut the cauliflower into chunks and use the medium-sized holes on a cheese-grater – to grate into “rice.” This process can also be done using a food processor.
- Transfer “rice” to a paper towel and press and squeeze to remove any excess moisture and leave to one side.
- Fry in a large frying pan over medium heat in a little oil. Cover with a lid so the cauliflower steams and becomes more tender. Cook for a total of 5-8 minutes, then season as desired (leave this step until the curry is almost ready).
For the Chicken & Lentil Curry
- In a large pan or saucepan, on a medium heat, warm some oil or low calorie-cooking spray.
- Add the onions and cook for 5-minutes, until soft and lightly browned.
- Add the chicken and cook for a couple of minutes until seared.
- Stir in the garlic, ginger and spices and allow them to release their fragrance.
- Add the tomatoes, stock and bay leaves and simmer for 35-minutes until the chicken is tender and the lentils have broken down.
- Remove the lid for the last 10-minutes and at this point start with the mushroom bhaji and cook the cauliflower rice.
For the Mushroom Bhaji
- In a separate pan, warm a little oil or low-calorie cooking spray. Add the onions and cook until soft.
- Add the mushrooms, ginger and garlic and cook until the moisture has evaporated.
- Add the spices and cook for 1-minute so that they release their fragrance.
- Add the tomatoes and about 50ml of water to loosen the mixture. Cook until the tomatoes have broken down.
- Serve with some plain yogurt and coriander.
Smokey Chipotle Chilli Tacos
This incredible taco recipe uses high-protein beans with low calorie lettuce tacos which makes this an amazing alternative to a chilli con carne and nachos.
This meal is high-protein, low fat and provides under 440kcal per portion.
Ingredients (serves 4):
For the Chilli – 1 stick celery, 1 large onion, 1 red pepper, 2 cloves garlic, 2 red chilli’s, 3 tsp chipotle paste, 400g canned kidney beans, 400g canned black beans, 400g canned pinto beans, 400g chopped tomatoes, 500ml vegetable broth, 1 bay leaf, 1sp ground cumin
To Garnish – 4 spring onions, 4 tbsp greek yoghurt, 1 lime, 1 handful chopped coriander
To Serve – gem lettuce, used as tacos
Nutritional Information (per serving)
Calories 436, Fat 6.3g, Carbs 72.9g (11.7g of which sugars), Fibre 23.3g, Protein 26g
For the Chilli
- In a large pan or saucepan, on a medium heat, warm some oil or low calorie-cooking spray. Add sliced onions, pepper and celery and cook for 5-minutes, until soft and lightly browned.
- Add sliced chilli and crushed garlic and cook for a further 3 minutes.
- Add the cumin and cook for 1 minute until it releases its aroma. Then add the chipotle paste and mix in.
- Drain and wash all the beans and add to the mix. Allow the beans to cook for a few minutes – it’s ok if they start to break up as this will thicken the chilli later.
- Add the tomatoes, stock and bay leaves, cover with a lid and simmer for 35-minutes until the chilli is thick and aromatic.
- Top up with a little water now, if the chilli is looking too thick.
- Garnish with some plain yogurt, sliced spring onions, coriander and lime.
- Dig in with some individual lettuce ‘tacos’.
Southern Fried Chicken & Sticky Cauliflower Wings
This indulgent recipe uses high-protein chicken with an array of spices for a real taste of the south, accompanied by moreish cauliflower ‘wings’ makes this a finger-licking dish that any colonel would be envious of.
This meal is high-protein, low GI and provides 187 kcal per portion and only 14.2g carbohydrates.
Ingredients (serves 4):
For the Spiced Chicken – 1 tsp paprika, 1 tsp cajun spice mix, 1 tsp dried thyme, 1 tsp dried oregano, 1 tsp garlic powder, 400g chicken breast
For the Cauliflower ‘Wings’ – 1 head cauliflower broken into florets, 2 tsp chipotle paste, 2 tsp tomato puree
Nutritional Information (per serving)
Calories 187, Fat 3.4, Carbs 14.2g (6.2g of which sugars), Fibre 6.3g, Protein 26.1g
For the Spiced Chicken
- In a small bowl mix all the spices together until well combined.
- Spread some tin foil on the counter – enough to wrap the chicken a couple of times.
- Place the chicken on the foil and cover top and bottom with the spice mix.
- Wrap the chicken in the foil to create a little parcel.
- Take a rolling pin and bash the chicken in the foil all over until flattened. You might burst the foil in places.
- Unwrap the chicken, it should be about 1-2cm thick throughout.
- In a large pan or saucepan, on a medium heat, warm some oil or low calorie-cooking spray. Add the chicken and cook until it is white throughout.
For the Cauliflower Wings
- Break the cauliflower into individual florets.
- In a bowl, coat the cauliflower in chipotle paste and tomato puree.
- Roast in the oven on 200c for 20 minutes, or until tender with a little bite.
Chinese Sweet & Sour Turkey & Stir Fried Vegetables
This incredible Chinese style stir fry uses delicious turkey with a rainbow of vegetables which makes this an great alternative to a Chinese takeaway.
This meal is high-protein, low GI and provides 378 kcal per portion.
Ingredients (serves 4):
1 tbsp soft brown sugar, 1 tbsp vinegar, 150ml chicken stock, 1 tsp tomato puree, 1 tsp Chinese five-spice, 1 tsp flour, 400g turkey escalope sliced, 2 cloves garlic, 2 peppers (any colour), 2 spring onions, 1 tsp ginger, 200g broccoli florets, 200g carrots, tin water chestnuts or bamboo shoots, handful cashews
Nutritional Information (per serving)
Calories 378, Fat 19.2g, Carbs 33.5g (7.7g of which sugars), Fibre 4g, Protein 18.1g
To make the sweet and sour turkey & stir fry vegetables
- In a large pan or saucepan, on a medium heat, warm some oil or low calorie-cooking spray. Add sliced turkey and lightly brown.
- Add broccoli and sliced carrots and cook lightly until slightly softened.
- Add garlic, peppers, spring onion and ginger and cook until aromatic.
- Drain and wash the water chestnuts (or bamboo shoots) add to the stir fry.
- In a separate pan, mix all the ingredients together except for the flour.
- Once mixed together, add the flour and stir quickly to combine allow to simmer gently and the mixture should thicken.
- Once at desired consistency, add to the turkey and vegetables.
- Garnish with cashews for some extra crunch.
At Spirit Pharmacy we’re here to help people live well with diabetes. We offer a free NHS prescription delivery, expert support, plus we have an online shop with healthy eating and diabetes products.

In our very first edition of our Diabetes Treatment “Need to Know” series, and as part of our focus on mental health, Roma, the newest pharmacist to join the Spirit Pharmacy family, talks us through everything you need to know about taking anti-depressants when living with diabetes.
Is there a link between diabetes and depression?
Yes, there is. According to NICE (National Institute for Health and Care Excellence), depression is three times more common in patients with diabetes.
You may feel overwhelmed in managing your diabetes, its complications or simply knowing that the condition is long-term. You may feel restricted in eating your favourite foods, feel obliged to take diabetic medication regularly, or often experience symptoms that affect your quality of life.
These are some factors that may occasionally cause a low mood, but if you start experiencing long periods of sadness, it is important to see a healthcare professional to rule out depression.
What are the most common anti-depressants people with diabetes are likely to be prescribed?
Medication is not actually the first step to treat depression. If you have mild to moderate depression, your doctor is initially likely to recommend lifestyle changes, such as exercise, mindfulness, counselling, and cognitive behavioural therapy to encourage self-help.
If these are ineffective, or if you have moderate to severe depression, then your doctor is likely to recommend medication. There are three main classes of anti-depressants.
Which anti-depressant your doctor prescribes will be dependent on your personal medical history, any existing conditions and what may work for you. The most common examples of anti-depressants include sertraline, fluoxetine, citalopram and duloxetine.
Are there any dangers to taking anti-depressants alongside my diabetes meds?
Anti-depressants and diabetic medication are safe to take together. However, anti-depressants can interact with other medication, such as ibuprofen, so I highly recommend reading the patient information leaflet for your anti-depressant to know which medication to avoid.
Anti-depressants can have several side-effects, which may appear similar to the symptoms of a hypo in diabetes, or to side effects of common diabetic medication, such as indigestion, dizziness or feeling shaky, so it is important to keep up-to-date with your regular diabetic checks.
Please be patient with anti-depressants as it can take two to four weeks before you feel any better!
Can anti-depressants affect my blood sugar levels or increase the risk of a hypo?
Studies have been conducted on certain anti-depressants which have suggested there may be a possible link between their long-term use and the risk of developing type 2 diabetes, but there is little evidence to suggest that anti-depressants directly cause a rise in blood sugar levels.
If your healthcare professional feels that a particular anti-depressant may not be suitable for you, then they will prescribe a different type as there are many options.
And with your regular diabetic checks, any fluctuations in blood sugar levels will be detected by your healthcare professional and appropriate action would be taken.
I often feel down due to my diabetes but am reluctant to go on to anti-depressants. What should I do?
I would advise speaking to your doctor and explaining your concerns. Based on your personal situation, the doctor is likely to recommend non-medicinal treatments at first, such as exercise and psychotherapy. If necessary, they may suggest anti-depressants.
Treating depression when you have diabetes is important as it can otherwise make it more difficult for you to manage your diabetes both physically and emotionally, as depression can heavily affect your choices.
For example, you may choose to comfort eat or skip meals, or prefer not to exercise when feeling low. These decisions could lead to poor blood sugar control over time.
Is there anything else you’d recommend for people who live with both diabetes and depression?
Dealing with diabetes can understandably cause feelings of stress, anxiety and low mood as it places emphasis on long-term diet and lifestyle changes, regular blood tests and adherence to medication.
If you feel overwhelmed and you need help, I would highly recommend asking your healthcare professional. A lot of people can feel anxious to start on a new anti-depressant but please don’t fear taking this step if necessary.
Ultimately, medication is there to help you. Any issues or concerns regarding side effects can be addressed by your healthcare professional and diabetes support groups are also available. You are not alone!
Thanks for lending us your expertise, Roma! Look out for the next edition of “Diabetes Treatment – “Need to Know”, where we’ll delve into common diabetes treatments & medications, explaining the top things you should know about them.
At Spirit Pharmacy we’re here to help people live well with diabetes. We offer free NHS prescription delivery, expert support, plus a free Live Well With Diabetes welcome pack with your first delivery.
Please note, this article is not intended to be individual healthcare advice. Always follow specific advice relating to your condition given to you by your doctor, pharmacist, diabetic nurse, or dietician.
Being diagnosed and living with diabetes is a stressful experience, and in addition to external factors like work-related stress, relationship or financial worries, or day-to-day things like children driving you up the wall or your daily commute, stress can have a real and serious impact on your health. This can affect your blood sugar levels as cortisol (the stress hormone) releases extra glucose into the bloodstream. Here are nine ways to reduce stress for better blood glucose control
- Reduce Caffeine
Studies show that drinking coffee (and to a lesser extent, tea) increases the stress levels in your body and releases cortisol, which increases blood sugar levels. Try to reduce caffeine gradually and look for decaf alternatives or herbal teas.
- Regular Exercise
Research shows that participating in regular physical activity can increase insulin sensitivity and assist with lowering blood glucose levels, as well as burn calories. For beginners, it is recommended to build up to 150 minutes of moderate aerobic activity, such as jogging or brisk walking, each week. You can even do home workouts or use online exercise videos if you do not want to go to the gym.
- Get Enough Sleep
A good night’s sleep supports your body and mind to tackle day to day stress more easily. If you are tired you can be less patient and more easily agitated which can increase stress. Most adults need 7 to 9 hours of sleep each night. Practicing stress-lowering tactics can also help improve your quality of sleep.
- Get Organised
Putting in some extra effort of getting organised, especially if this organisation extends to multiple areas of your life, can help reduce stress levels long term by requiring less last-minute scrambling in a variety of everyday situations.
- Find Time for Creative Pursuits
Creative pursuits like art and crafts, creative writing or woodworking can help focus the mind, and has even been compared to meditation due to its calming effects on the brain and body. Even just gardening or sewing releases the natural antidepressant – dopamine.
- Take Time Out
Feeling like you’re on the go all the time? Too much work and not enough play can contribute to problems feeling stressed out, so taking some time out to relax is essential for your health and mental wellbeing. Making yourself the priority may make you feel selfish, but if you do it on a regular basis it can help to reduce your stress levels.
- Breathe
Your breath is a powerful tool to ease stress and make you feel less anxious. Some simple breathing exercises can make a big difference if you make them part of your regular routine. Take a deep breath in. Now let it out slowly. You may notice a difference in how you feel already.
- Talk About It
Talking through your worries and concerns with family and friends is an important buffer against stress. It can be helpful to share your problems with people who care for you. If you live with Type 2 diabetes, you can connect to other people who understand what it’s like living with the condition on our dedicated Facebook group.
- Good Nutrition
Reducing junk food and refined sugars that are low in nutritional value and high in calories can stop us from feeling low on energy and sluggish, not to mention being unhelpful for managing your blood glucose levels. A healthy, balanced diet that is low in sugar, caffeine, and alcohol, can promote good health and reduce stress.
At Spirit Pharmacy we’re here to help people live well with diabetes. We offer free NHS prescription delivery, expert support, plus a free Live Well With Diabetes welcome pack with your first delivery.
Please note, this article is not intended to be individual healthcare advice. Always follow specific advice relating to your condition given to you by your doctor, pharmacist, diabetic nurse, or dietician.
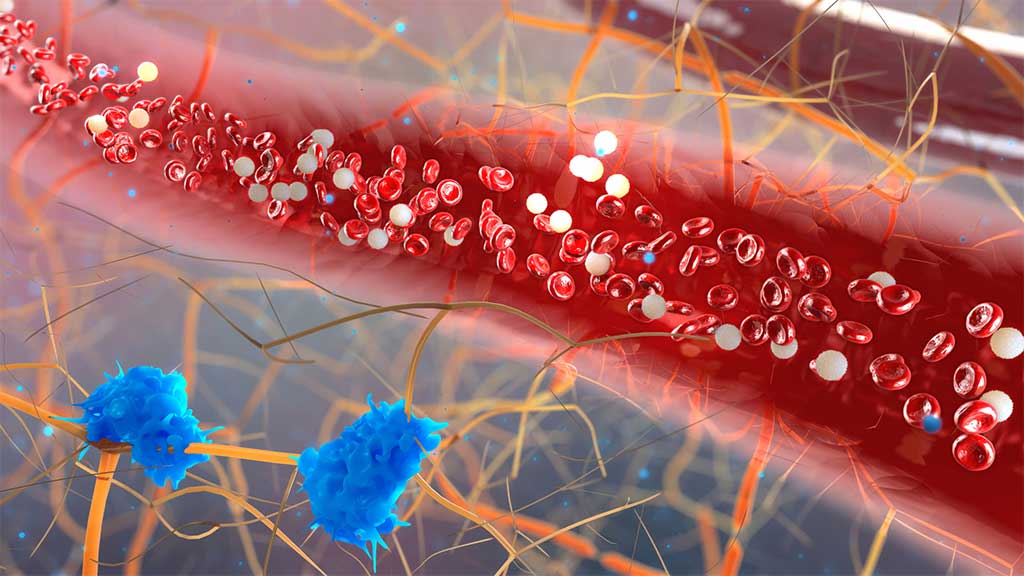
Blood glucose is a sugar that the bloodstream carries to all cells in the body to supply energy. If you have uncontrolled diabetes, your blood glucose level will tend to be higher than it should be. The aim of managing your levels is just to keep them in a healthy range.
What is blood glucose?
Your body creates glucose by digesting food before using it as a source of energy. As it travels in your blood stream to cells, it is called blood glucose. Your blood glucose level, also known as blood sugar, is the amount of glucose in your blood.
Most people’s levels stay relatively stable as their body maintains a normal range. However, if you have diabetes, your glucose level can fluctuate outside of ‘healthy’ ranges either peaking too high or, with some medications, dropping too low. High levels for a long period of time can damage your eyes and kidneys.
The importance of monitoring blood glucose if you have diabetes
A continuous high blood sugar level can damage your blood vessels, making it harder for blood to flow around your body. High levels can increase your risk of:
- Heart disease or heart attack
- Stroke
- Kidney disease
- Nerve damage
- Eye disease (also known as retinopathy)
How to check your levels

A standard test involves pricking your finger with a small needle called a lancet, drawing a drop of blood from your finger and applying it to a test strip that you use with a blood glucose meter.
Your meter measures your blood and shows you a numeric reading of the number of millimoles per litre (mmol/l).
Some people prefer to use a continuous monitor instead of pricking their fingers.
You should measure your blood glucose more frequently if you’ve made any lifestyle changes such as:
- If you’re ill and it’s affecting your usual eating habits.
- You have recently changed your diabetes medication.
- You have recently changed your meal plan.
- You have recently changed your level of physical activity or you are trying a new sport/exercise.
- If you’re experiencing a lot of stress.
If you take certain medicines for diabetes, such as insulin, it’s vital to regularly monitor your glucose level. It can help you know when you need to use your medication, when to move around and when you need to eat something to prevent your levels peaking or dropping.
Hypoglycaemia vs hyperglycaemia
What is a ‘good’ level?
NICE guidelines recommend the following for a ‘good’ blood glucose level in mmol/l:
- A normal level before a meal (called pre-prandial) will be between 4 and 7 mmol/l.
- After eating (post-prandial), levels should be below 9 mmol/l when tested 2 hours after a meal.
- When going to bed for the night, levels should be no more than 8 mmol/l.
What should you do if your blood glucose is high or low?
If your blood glucose does go out of range, it’s important to know what you can do to bring it back in line. Here are some tips:
- Drink plenty of water and stay hydrated.
- Control your stress levels.
- Get enough quality sleep.
- Exercise regularly.
- Control your carb intake and increase your fibre intake.
How Spirit Pharmacy can help you?
Spirit Pharmacy offers a friendly NHS prescription home delivery service. We love providing pharmacy services for everyone, but especially people with diabetes. Free services include prescription reviews and access to online diabetes education.
Order your medicines on the phone or online and we will post them to you safely with fast, free delivery. We post insulin in insulated packaging which can keep it cool for up to 3 days. We also can provide you with insulin passports, to help you keep record of your glucose levels, free diabetes education with can help you best manage your condition and our pharmacists are here to speak to if you have any queries or concerns! Get in touch today to see how we can help you!
Register hereClinical Content
https://www.diabetes.co.uk/diabetes_care/diabetes_and_blood_glucose.html
https://www.medicalnewstoday.com/articles/249413